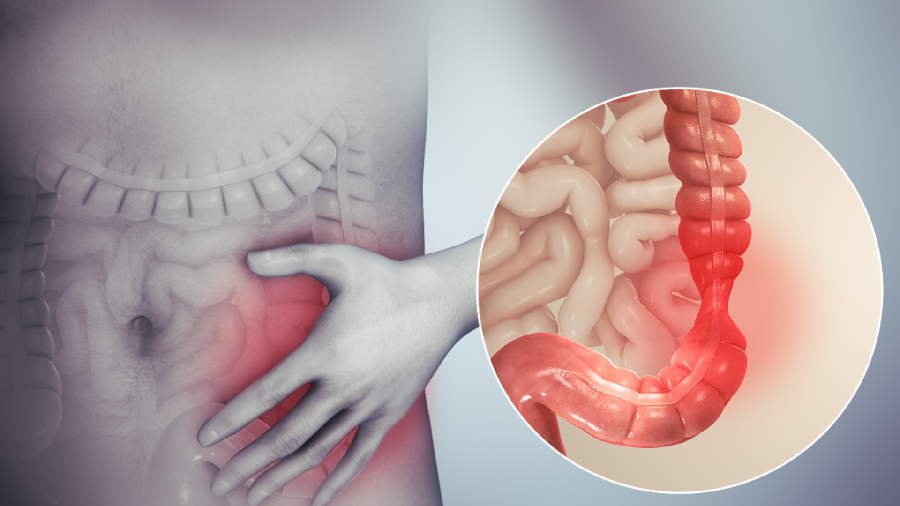
Irritable colon is a chronic pathology of unknown cause, characterized by abdominal pain or discomfort accompanied by episodes, generally alternating, of diarrhea and constipation in the absence of an identifiable disease in the intestine.
The frequency of symptoms is highly variable and their intensity, affecting both sexes (although more frequently women) at any age.
It is usually associated with other diseases included in the term functional somatic syndromes: fibromyalgia, chronic pelvic pain, headache, interstitial cystitis, etc.
What are the causes of irritable bowel?
The causes of irritable bowel are unknown. Some doctors think it is due to intestinal spasms (hence its other name, spastic colon). It occasionally appears after an intestinal infection and is often associated with anxiety or depression.
What symptoms does irritable colon cause?
The symptoms of the irritable colon are very varied, the most frequent being:
- Abdominal pain or discomfort. It is the key symptom, highly variable in its intensity and location. The pain or discomfort may be located in the lower abdomen (in, the lower abdomen), on the right side, on the left side, or in the stomach area. They are usually cramps, although there may also be continuous dull pain. The pain can be very mild or severe and can prevent you from leading an everyday life. It can increase with eating or stress, and, in women, it can grow with menstruation.
- Suppose it is an irritable colon with a predominance of constipation. In that case, the stools are usually complex, and the patient has the feeling of not having finished having a bowel movement, therefore going to the bathroom several times a day. In patients with irritable bowel in which diarrhea predominates, it is usually of little quantity and worsens with stress or food. Diarrhea may have mucus.
- Other frequent symptoms in all forms of the irritable colon are the feeling of a swollen gut and regular gas, heartburn, and heavy digestion, associated with nausea and vomiting.
How is it diagnosed?
There is no test to confirm the presence of an irritable bowel. To diagnose it, it is necessary to rule out other diseases that can produce similar symptoms (stomach problems, gallbladder problems, pancreas problems, lactose intolerance, adult celiac disease, other diseases of the intestine) for which, in addition to carrying out a detailed examination, they must request blood and stool tests and, on many occasions, other tests such as barium enema, colonoscopy, gastroscopy, etc.
Given the normality of these tests, the criteria for diagnosing an irritable bowel are:
- That the digestive alterations have been present for a minimum of 6 months.
- That there is recurrent abdominal pain or discomfort, at least three days a month, and that it is associated with at least 2 of the following data:
- Pain or discomfort improves with bowel movements.
- The onset of discomfort or pain is associated with a change in the frequency of bowel movements.
- The onset of pain or discomfort is associated with a change in stool consistency.
Forecast
Irritable colon is a chronic disease that evolves in outbreaks, frequently associated with situations or periods of special stress. There is no curative treatment, although treatments can improve symptoms. However, most patients with IBS have mild to moderate forms of the disease that respond reasonably well to treatment. Specialists should evaluate the few cases resistant to treatment.
What is the treatment for irritable bowels?
Irritable colon treatment includes the following aspects:
- It is important to explain that, although the disease is not serious, it can be very annoying. Available treatments can improve the disease, but none cure it. In general, several treatments are tried, alone or in combination, until the most effective is found.
- Diet recommendations. Some foods that precipitate an episode can be identified, such as coffee, legumes, cabbage, artificial sweeteners, etc. Therefore, it is important to research diet and foods that can cause an acute outbreak. In addition, any food that causes flatulence (carbonated drinks, legumes, green leaves, etc.) and those habits that can produce gas (chewing gum) can worsen some of the symptoms, so they should be abandoned. A low-lactose diet is often recommended for 2 or 3 weeks. If there is clinical improvement, it is reasonable to continue with it. On the contrary, if the disease remains the same, the low-lactose diet should be abandoned. In the irritable colon, some foods are especially well tolerated, such as:
- Water, sprite, isotonic drinks.
- Soy milk.
- Rice.
- Pasta without sauces.
- Roasted or boiled potatoes (not fried).
- Bread or muffins.
- Fish, chicken, ham without sauces.
- Eggs are prepared in any way except fried.
- breakfast cereals
- Lettuce salads.
- We cooked peas or carrots. Avoid raw vegetables.
- Margarine, jams, nocilla.
- Melon in small quantities.
- Peaches pears packed in small quantities.
Specific treatment recommendations are:
- A diet rich in fiber and the use of laxatives that increase stool volume: Psyllium (Plantaben, Metamucil) or methylcellulose (Muciplazma), are effective in some patients with irritable bowel syndrome, both in those with have constipation as in those with diarrhea. In some patients, a high-fiber diet can worsen flatulence and gas, so it is best avoided in these circumstances.
- To reduce abdominal pain or discomfort, antispasmodics such as mebeverine (Duspatalin), trimebutine (Proctolog), titanium (Spasmoctyl), scopolamine butylbromide (buscopina) are recommended. Several of them can have adverse effects, especially in the elderly.
- In irritable colon in which diarrhea predominates, astringent medicines such as loperamide (Fortasec) or resin cholestyramine are recommended.
- Tricyclic antidepressants have shown efficacy in some patients despite no data suggesting depression. They are used at much lower doses than would be used in depression. The mechanism of its effectiveness is unknown. Various other antidepressants (serotonin reuptake inhibitors) have also been effective in studies in which IBS was associated with depression.
- Some treatments with antidepressants or anxiolytics or psychological treatments have shown improvement in some people, generally in the forms that prefer diarrhea.
- Antibiotic treatment is not currently recommended, although some doctors believe that bacterial overgrowth within the intestine may play a role in this disease and give antibiotics.
- Other parapharmacy treatments have not shown efficacy so far. The use of yogurts with Bifidus-type bacteria is not useful. Peppermint oil and other oils commonly recommended to treat irritable bowel can even be dangerous in the long term by irritating the intestine and promoting electrolyte loss.